How Do I Know If I Have A Clogged Milk Duct?
A plugged or clogged milk duct (also called a blocked duct) usually feels like a hard, tender swelling in the breast which can vary in size from a pea to a peach and may feel painful while breastfeeding. The skin over the affected area may be red and the area around the plug may feel full even after a feeding. Sometimes a small whitish-yellow milk plug (bleb) can be seen at the opening of a duct on the nipple. Plugged ducts occur when milk flow is restricted, or there is a delay in removal of milk from the breast resulting in poor drainage of the breast.
Contributing factors to a clogged duct may include:
- Missed or irregular feedings and/or an unusually long interval between feedings (a sudden long sleep stretch).
- Pressing the breast to provide nostril space for the baby.
- Wearing a tight, poorly fitting, or underwire bra that impedes milk flow.
- Having an overabundant milk supply and insufficient breast drainage.
- A plugged nipple pore/nipple bleb (looks like a white head).
- Rapid weaning.
- Practicing vigorous upper arm exercise.
- Extreme exhaustion.
An untreated plugged duct can quickly lead to a painful bacterial infection in the breast called mastitis. These latest updated tips can help you clear the plug and avoid the onset of mastitis. If there is no change in your breast in two days, or you begin to notice signs and symptoms of infection, notify your obstetrician. Antibiotics may be indicated.
Treatment suggestions for a plugged duct: follow this plan every 2-3 hours until the plug is relieved.
First: Gentle Lymphatic Drainage Massage
- The purpose of lymphatic drainage massage is to drain inflammatory fluid from the breast gland to the lymph nodes at the neck, clavicle and armpit.
- Lightly massage - like petting a cat - the breast from the nipple past the plug and outwards towards the clavicle, armpit and neck.
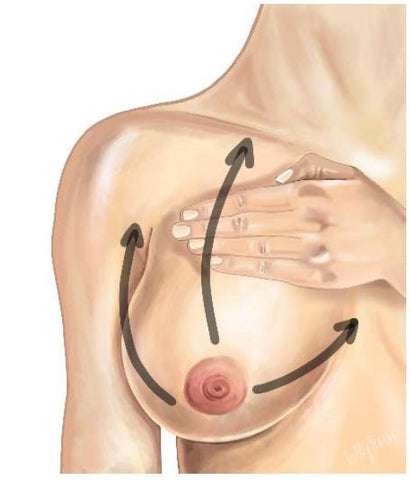
- Work in 3 quadrants, starting at the nipple and working out towards your armpit for 1 minutes, then out from the nipple towards your clavicle for one minute and then out from the bottom of your breast towards your neck for one minute.
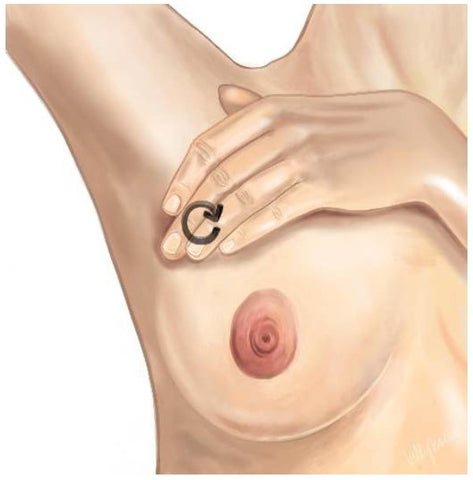
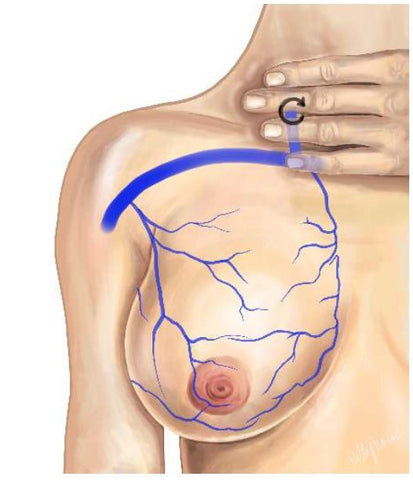
- IF you use vibration, use it LIGHTLY over the plug and outwards towards the neck and clavicle or axilla depending on what part of the breast is inflamed.
Images used w/ Permission from: Dr. Katrina Mitchell, MD, Physicians Guide to Breastfeeding
Second: Nurse your baby or Pump
- Nurse or pump (whichever you’re doing to relieve the breasts) every 2 to 3 hours.
- Do not miss any feedings.
- Make sure the baby is deeply latched.
- Start each nursing on the affected breast. If using only one breast at a feeding, nurse on the side with the plug at each nursing and pump the other breast as frequently as you would have nursed on it.
Third: Ice/Pain Relief
- A plug is not just a source of milk plugging, it is also an area of inflammation. It is helpful to ice the area after relieving with nursing/pumping.
- Take anti -inflammatory medications, Advil or Motrin, as directed on the bottle for pain and inflammation.
Fourth: High quality probiotic specific to breast health
- Elactia: Elactia is a probiotic specifically formulated for breastfeeding parents.
- The probiotic. L. fermentum, can ease breast discomfort and promote a healthy bacterial microbiome in the breast
Additional Strategies to Help Relieve the Plug:
- Vary nursing positions. Have the baby's nose or chin pointed toward the plug.
- If a bleb/plug appears at the nipple (looks like a cheesy whitehead), place a cotton ball soaked in warm olive oil against the nipple bleb for 5 minutes to soften the plug. Gently rub the plug to remove the top layer of skin, and then try to massage the plug out.
- Use gravity to help move the bleb/plug by nursing on all fours with the baby on pillows below you.
- Increase your fluid intake.
- Increase your intake of Vitamin C rich foods and juices (citrus, cantaloupe, strawberries, dark greens)
- A homeopathy remedy may be helpful: Phytolacca 30 C &/or Silicea 10 C. Take one dose (3-5 pellets under the tongue) at onset. Wait 30 minutes. If no change or slight improvement repeat the dose and again wait 30 minutes. If there is no change at all after the second dose STOP as this is likely not the right remedy for you.
- If you DO see improvement then repeat the 3-5 pellet dosage in 3- 5 hours.
- Consider acupuncture/acupressure or Chinese herbology.
- Therapeutic ultrasound can be helpful in breaking up the blockage. One treatment is usually sufficient, but occasionally a second visit or more is required. Dr. Jack Newman of the International Breastfeeding Centre suggests that if two treatments on two consecutive days have not resolved the blockage, more treatments will not be effective and you should see your physician.
-
Castor Oil compresses can relieve pain, reduce inflammation, and aid in removing persistent plugs (do not use on broken skin).
- Use a high-quality, cold-pressed Castor oil (available at most natural food stores).
- Take a large piece of cotton (a piece of an old t-shirt or a flannel cloth) sized to cover the plug. Fold three times for thickness.
- Saturate flannel with Castor oil and warm in the microwave—beware of hot spots—wring it out so that it remains wet but not dripping.
- Apply the cloth to the plugged area of the breast.
- Cover with plastic wrap and then apply heat (a hot cloth, heating pad, hot water bottle, etc.).
- Keep in place for 20 minutes.
- After treatment, rinse the breast so the baby does not ingest the castor oil, then pump or feed the baby.
- Repeat treatment 2-3times/day. Plug often resolves within 24 hours.
- The flannel pack can be reused several times. Place it in a bag for future use. No need to wash—it can be used as is. If it dries out, more castor oil can be added.
-
Soy/Sunflower Lecithin:
- For repeated plugged ducts, some women find that soy or sunflower lecithin is helpful in lessening the chance of a recurrence.
- Sunflower lecithin is a naturally occurring fatty acid. It is available in capsule form at The Pump Station and Nurtury as well as some health food stores and pharmacies.
- The recommended dosage is 1 capsule (1,200 milligrams each), 3 to 4 times/day until there is no further plugging.
Mastitis
When Mastitis develops, the woman's symptoms worsen. The plugged area of the breast becomes hot and the redness increases. The mother usually feels very sick and has a fever with body aches, chills and a headache, very similar to the flu.
Treatment Suggestions for Mastitis:
- Continue following the suggestions listed above for a plugged duct.
- Call your physician immediately and take the prescribed antibiotic for the duration required by your doctor. You should start to feel better within 24 to 48 hours. If not, call your doctor. He/she may want to change your medication.
- Mother and baby should both take probiotics while mother is taking antibiotics. Probiotics help maintain a healthy intestinal flora and lessen the chance of developing a yeast infection.
- Most physicians agree that acetaminophen (Tylenol 650-1000 mg) and Ibuprofen (Advil or Motrin 400 mg) are helpful for reducing pain and fever. Ibuprofen also helps reduce inflammation. Try alternating these medications every 3 hours; for example: take acetaminophen at 6-12-6-12 o’clock and Ibuprofen at 3-9-3-9 o’clock. Always check with your doctor before starting any medications.
- Sometimes the breast becomes is hard, hot and swollen, and some babies struggle to latch and become frustrated during feeding. If this happens, pumping is necessary to protect milk supply. A hospital grade, electric breast pump is suggested and may be more comfortable than breastfeeding.
- Mastitis can occasionally lead to a breast abscess. This is a pocket of pus that forms within the infected area of the breast. Abscess formation is actually the body’s defenses at work to localize an infection and keep it from spreading. Let your physician know if the lump in your breast does not go away, even if your other symptoms are improving.
More Pump Station blog topics:
When should I offer a breastfed baby a bottle? Click to read
Is baby crawling still regarded as a developmental milestone? Read this
How To Achieve A Deep Latch - click here
Check out our entire Breastfeeding Help Library here
Copyright© 2024 by The Pump Station & Nurtury®. All rights reserved. No part of this may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, without permission in writing from The Pump Station & Nurtury®. This article has not been prepared by a physician, is not intended as medical advice, and is not a substitute for regular medical care. Consult with a physician if medical symptoms or problems occur. (Revised 10/14/24)























