Low Milk Supply
In the United States, concern about low milk supply is the most common reason given by women for supplementation and early weaning. Why do so many women in our culture lack confidence in their ability to adequately nourish their babies? Sociologists believe, that during the last century, the decline in breastfeeding contributed to the loss of knowledge about how breastfeeding really works, and how breastfed babies behave.
- It is normal for women to feel that they don't have milk in their breasts the first days after birth. Frequent breastfeeding during this time will meet the new baby's need and cause the milk supply to increase rapidly.
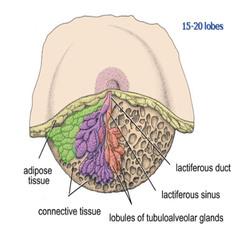
- A good milk supply is encouraged by frequent sucking and effective removal of milk. If milk is not being removed from the breast, the supply will not increase, but instead drop. If a baby needs more milk he will usually nurse more frequently which causes the hormone Prolactin to rise and the milk supply to increase.
- New research shows that although almost all women can produce plenty of milk, some women need to nurse more often than others in order to meet their baby's caloric need.
- A baby needs to be latched deeply onto the areola, not just the nipple, to effectively remove milk.
- Human milk passes through the baby's stomach in 48-90 minutes. The breastfed newborn needs to nurse 8-12 times/24 hours, while the formula fed baby feeds only 6-8 times/24 hours. If a breastfeeding mother tries to feed her baby on a bottle schedule, her baby may not get enough food.
- A baby will often need to be held, rocked, jiggled and bounced (just as in the womb) even after a good feed. Babies cry for reasons other than hunger. Don't worry about "spoiling" a newborn by holding him too much. If a baby's needs are met, trust is built and good self-esteem and independence will follow.
- Young babies have a 3-hour wakeful stretch every day, during which they want to be at their mothers' breast the majority of the time (the marathon feed). This usually occurs in late afternoon/evening and is normal.
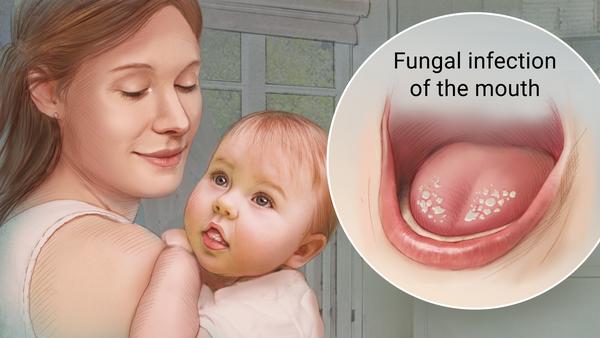
- Difficult or poor latch-on that leads to poor milk removal. If a baby cannot sustain attachment to the breast for more than a few sucks or if he is only on the nipple, he cannot remove milk and is not nursing well.
- Early introduction of a bottle. If given formula, the baby won't need to breastfeed often and decreased breast stimulation will generally result in a decreased milk supply. If your doctor advises supplementing your baby, check with a lactation consultant for extra guidance in protecting and maximizing your milk supply.
- Babies set their own schedule and some need to eat more often than others. Research indicates that a mother needs to be responsive to her particular baby's lead and not adhere to a rigid plan.
- A sleepy, non-demanding baby. Make sure the baby is coming to the breast 8-12 times in 24 hours. Once weight gain is established, relax and follow the baby's lead.
- Anything that keeps a baby from nursing vigorously (jaundice, prematurity, illness).
- Augmentation and reduction breast surgery are both possible risks for a low milk supply. A lactation consultant can help devise a plan to maximize milk supply.
- A woman who has absolutely no breast changes during pregnancy or during the first week after birth may be at risk for a low supply. Seek extra advice from a consultant.
- Reduced breast stimulation as a result of: (next li Long Sleep... should be nested)
- Long sleep stretches by the baby
- A mother's busy lifestyle
- Insufficient rest due to a mother's return to the workplace
- Introduction of alternate baby foods
- Hormonal contraception. Even the "mini" pill causes some women's milk supply to drop dramatically.
- Pregnancy
- Excessive exercise and/or dieting
- Improve the baby's latch.
- Increase breast stimulation:
- Add more feedings and/or nurse longer. Wake the baby for feeds if necessary. Unwrap and undress to help waken.
- Use a good quality breast pump (hospital grade) and follow most breastfeeds with a 15-minute pumping session. Be patient, it may take a few days or longer to see results.
- While nursing on the second side, pump the breast the baby just finished (third breast pumping). This effective technique saves a lot of time.
- Switch sides. When the baby gets sleepy, remove from the breast, burp and switch to the other side. Repeat until the baby won't nurse anymore.
- Try herbal supplements: Mothers Milk tea, Fenugreek capsules (3 capsules 3 times daily), and Fennel seeds (crushed and made into tea, or just chewed). The effectiveness of these remedies is anecdotal, not research-based, but many mothers find it very helpful.
- Eat a well balanced diet with lots of whole grains and increase your fluid intake.
- Ask your OB/GYN to help you choose a non-hormonal contraceptive method.
- See a lactation consultant for an in-depth evaluation and strategies for improving your milk supply.
- Ask your doctor to prescribe Reglan or Domperidone (Motillium). These medications are usually used for gastric problems but have a side effect of raising the level of the hormone that increases milk supply. Domperidone must be made by a compounding pharmacy.
The Pump Station & Nurtury® has decades of experience providing new families with outstanding educational, breastfeeding and baby care support, including products and classes which can make all the difference to you and your baby. To see a list of some of the essential products that our Lactation Professionals have recommended, click Essential Breastfeeding and Baby Care Products
Products to help increase milk
See Other Breastfeeding and Baby Care Help Topics
Copyright©2017 by The Pump Station & Nurtury®. All rights reserved. No part of this handout may be reproduced in any form without permission from The Pump Station. This article has not been prepared by a physician, is not intended as medical advice, and is not a substitute for regular medical care. Consult with a physician if medical symptoms or problems occur. Revised 01/06